Medical professionals could potentially one day identify veterans with post-traumatic stress disorder (PTSD) through a quick blood test instead of complex psychological tests, thanks to new research from the
US Army and outside biometrics experts.
The study, which appeared in the journal Molecular Psychiatry, found a set of 27 blood markers which helped identify patients suffering from PTSD.
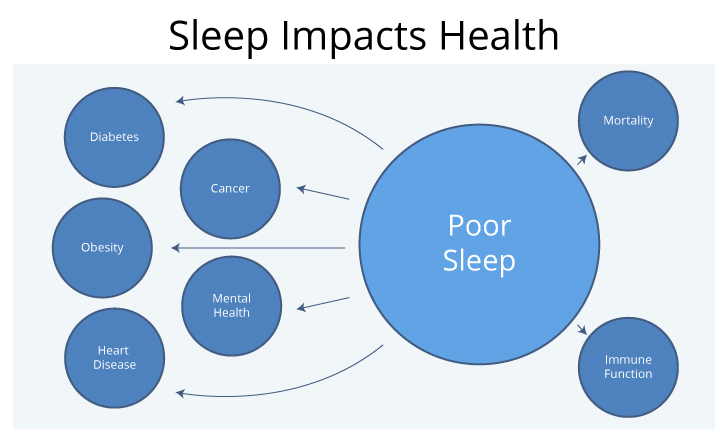
Researchers said the findings support past hypotheses that the disorder “affects not just the brain, but the entire body.”
In a statement, US Army Medical Research Systems Biology Chief Scientist Marti Jett said those markers “will continue to be refined and adapted for commercialisation” in coming years.
Researchers are hopeful blood tests can lead not only to more accurate diagnoses but also earlier ones, perhaps indicating signs of problems even before PTSD has fully manifested.
Senior study author Dr. Charles Marmar, chair of the Department of Psychiatry at the New York University School of Medicine, said a blood test could indicate signs of PTSD that veterans are unaware of or deliberately hiding out of fear surrounding the stigma of the diagnosis. It could also more quickly eliminate PTSD as a potential problem for patients with unclear medical issues.
“This is an attempt to take the field of psychiatry from the subjective to the objective,” he said. “It’s a way to start a new conversation about how to find the invisible wounds of war.”
But the study has limits. No women were among the veterans tracked for the research, and no civilians were included. Marmar said creating a simple, inexpensive blood test for widespread use to help diagnose PTSD is likely still years away. But he still lauded the findings as an important medical breakthrough for health experts looking for ways to more accurately track troops’ health.
Defence Department and Veterans Affairs researchers have estimated that as many as 25% of individuals who served in combat zones in Iraq or Afghanistan may suffer from PTSD, marked by uncontrolled anxiety, confusion or anger.
Officials have spent years trying to break down the stigma surrounding the diagnosis, which many service members fear could render them undeployable or otherwise unfit for duty because of the non-physical nature of the symptoms.
The study, the culmination of six years of work, tracked blood samples from 165 veterans, half of whom suffer from PTSD following deployments into war zones.
Scientists studied their medical histories and biochemistry, trimming down the list of potential identifying characteristics in their blood from more
than 1 million to less than 30.
In subsequent tests with other patients, the final set of blood markers showed a 77% accuracy rate in helping identify PTSD. Marmar said that is more than enough for a potential screening test, where medical professionals can follow up with more in-depth
examinations to diagnose the illness.
Past studies have hinted at blood markers as a potential indicator of PTSD, but researchers in the new study which included the Harvard John A. Paulson School of Engineering and Applied Sciences and the US Army Medical Research and Development Command said this is the first time a coherent set of measures has been developed.
Jett said that any screening tool that comes from the research would be used before and after deployments, and treatment for those issues would be provided based on military medical standards.
The full study is available on the journal’s website @ https://www.nature.com/articles/s41380-019-0496-z.







You must be logged in to post a comment.